It is a fear that afflicts us all, commonly voiced as “I don’t want to lose my marbles”.
Yet with an ageing population, the number of individuals living with dementia is rising.
Around a million people in the UK have a diagnosis, with over 50 million affected worldwide. It is estimated that these figures will triple by the year 2050. Alzheimer’s Disease (AD) is the commonest form of the condition, accounting for seventy percent of cases.
The onset of dementia is variable, from a state of normal cognition, through mild cognitive impairment (MCI), to dementia, a disease which robs persons of their identity, memory and often the ability to comprehend and carry out basic tasks.
The stage between MCI and full-blown disease is not set in stone, the good news being that some individuals will not progress beyond this stage.
The pathology associated with the development of Alzheimer’s Disease is the laying down of amyloid and tau protein, the latter causing the classic appearance of 'neurofibrillary tangles' seen on brain scans. These essentially interfere with normal brain tissue. With time, amyloid builds into clumps, referred to as plaques. However, brain scanning has shown that some individuals with amyloid deposition do not have cognitive impairment, and a third process, neuroinflammation, or simply inflammation of the brain, is also needed for progression to actual disease. While inflammation is a normal part of the body’s defence mechanisms, excess can harm this delicate balance.
Though many bemoan the lack of progress (it is commonly said there have been no real breakthroughs in dementia care for 20 years) development of diagnosis and treatment is rarely if ever linear, and sometimes a lag period is followed by an explosion of understanding.
Such has been the case with Alzheimer’s. Recent research has focussed on how amyloid gets laid down in the brain. Previously it was assumed that it was formed within the brain itself. However, lately it is understood that amyloid produced in the liver is transported in the blood to the brain, leaking through blood vessels at this site. Studies in mice showed that increasing the liver’s production of amyloid resulted in the development of memory issues and reduced functioning. Hence increased liver health may be one of the keys to lowering your risk.
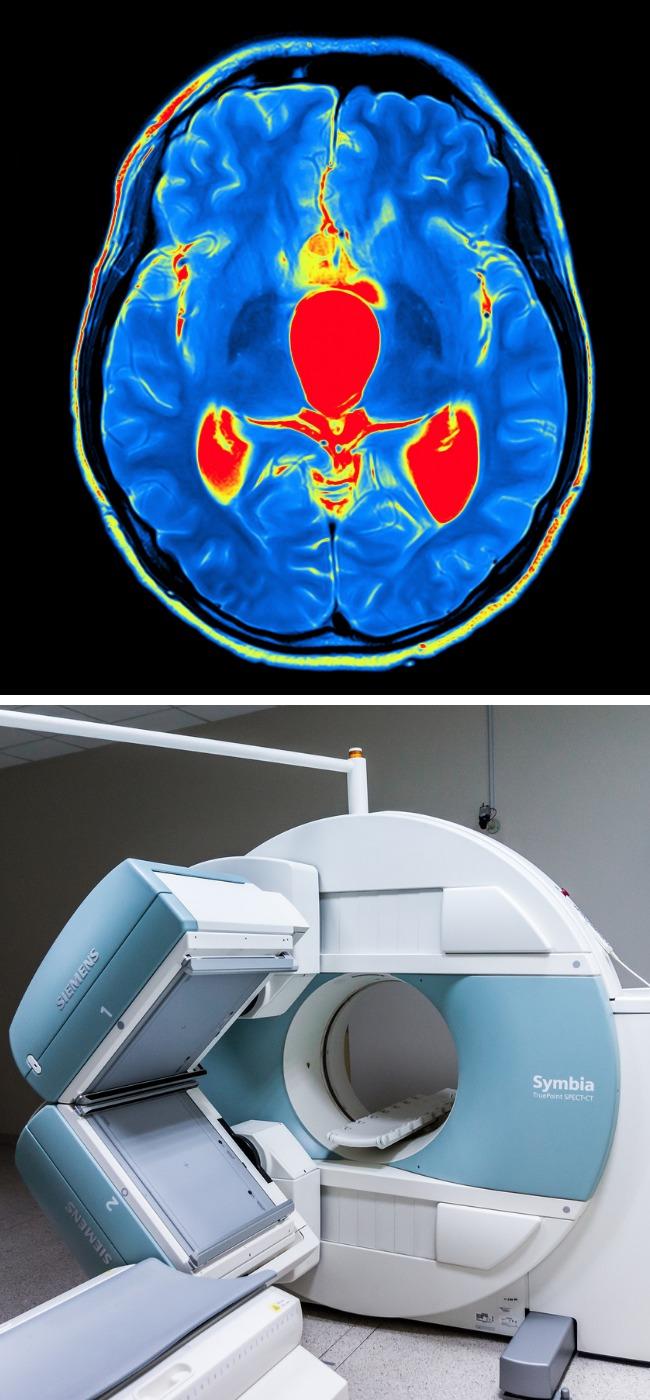
The workup of any memory condition usually includes a brain scan, either MRI or CT, which looks for classic appearances of disease, as well as signs of any other conditions which may be causing symptoms.

An MRI brain scan may be able to detect early signs of Alzheimer's. Picture: PA/ Thinkstock
The phase of MCI is often a difficult time, with many individuals naturally reluctant to come forward. However functional MRI has been shown in a small study to be able to pick out the subtle changes of this 'pre-Alzheimer’s' with almost one hundred percent accuracy. Early diagnosis is beneficial, so if this becomes mainstream, many may be helped in the early stages.
Preventing the build up of amyloid plaques or removing them from the brain will hopefully be one of the ways of preventing, halting or potentially reversing any cognitive decline. The American Food & Drug Administration (FDA) has recently approved the medicine aducanumab, a monoclonal antibody, which mimics the body’s natural antibodies, part of the immune system. Although further studies are needed, any drug that can remove amyloid plaques shows promise.
Many drugs have been trialled with limited success, including those to treat the cardiovascular system and diabetes. Yet the pathology that causes the development of Alzheimer’s Disease and vascular (blood vessel) disease, are the same; that being excessive inflammation.
The risk of Alzheimer’s, and indeed any dementia, is increased in those with cardiovascular disease. Alzheimer’s may also coexist with other forms of dementia. Any additional insult to the brain, be that through mixed dementia, or a stroke due to uncontrolled high blood pressure, will magnify the severity of symptoms, and reduce time to death.
Naturally, prevention is better than cure. Reduction of cardiovascular risk factors is twofold. Lifestyle measures include regular moderate exercise, and smoking cessation, alcohol reduction and weight loss, if applicable. Raised blood pressure and elevated cholesterol are often silent for many years, while damage is steadily accumulating, and I would encourage everyone to attend for regular blood and blood pressure checks as appropriate.
Some useful websites:




Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules here