HOW can we improve access to GPs as we move out of lockdown? York's two MPs go head to head and give their diagnosis on what's going on in primary care - and offer a prescription for improvement...
Julian Sturdy, Conservative MP for York Outer

Julian Sturdy
The government must also progress rapidly on its commitment to recruit 6,000 new GPs"
WHILE York’s GPs have done an amazing job arranging vaccination, and continuing to attend to residents throughout the pandemic, it is clear that a number of people have found it hard to access local medical attention.
Having already raised the matter with the leadership of Vale of York NHS CCG, the local umbrella body for GP practices, in February following feedback from a concerned elderly resident, I have now tabled parliamentary questions to the Health Secretary pressing him on the impact of emergency Covid triage arrangements on access to face-to-face GP appointments across the city. I have also lobbied the leadership of Vale of York NHS again in response to recent concern.
Thankfully, NHS England have last Thursday clarified the situation, with a revised standard operating procedure reiterating that practices should offer face-to-face appointments, which I hope will reassure York residents on this point. However, it is important to be clear that GPs have offered conventional in-person appointments throughout the pandemic when judged necessary, with half of consultations now face-to-face, down from 70 per cent pre-Covid.
READ MORE: "NHS is closed" Patients give verdicts on GP appointments in York
Read more: Can't get a GP appointment? What's going on at doctors' surgeries in York
READ MORE: "The doctor will see you now" - government announce U-turn on GP appointments
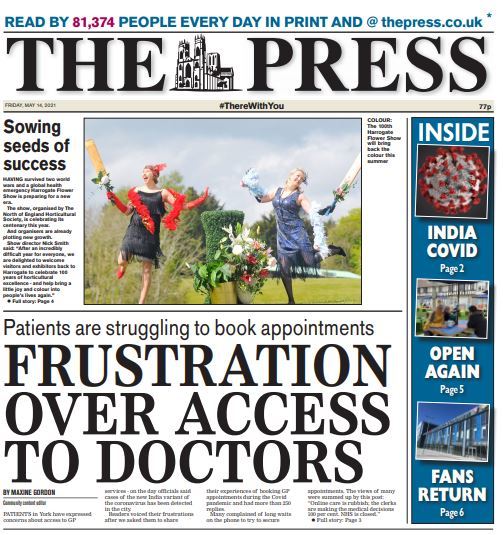
GP appointments - patients face delays, from The Press' front page on Friday
As these figures suggest, telephone and online appointments were already an important feature of GP care before the pandemic, and it is valuable for our health service to be able to draw on this technology to support those with busy working lives, and maximise the number of patients that can be seen.
Covid, and the need for strict infection-control procedures such as waiting-room closures, disinfection of consulting rooms after each appointment, and regular changes in protective equipment by practice staff, reduced the number of consultation slots. The pandemic also made it essential to minimise the risk of transmission by seeing patients remotely wherever possible, hence the extension of telephone and online services to be the resident’s first ‘point of contact’, after which a physical appointment could be scheduled when needed.
However, this system was not intended to prevent those requiring normal appointments from receiving them, and it should be a cause for serious concern and a rethink if this has been the case. Understandably, we won’t hear from the many residents who have appreciated a convenient and prompt telephone or online consultation, but recent alarm suggests the emergency procedures have not always been effective in ensuring everyone has received a service matching their medical requirements.

GP appointments - patients want easier access to doctors
Fundamentally, we need to strike the right balance between allowing GPs to use new methods to reach people wherever appropriate, and maintaining a universal service that does not exclude older or less tech-confident residents.
The government must also progress rapidly on its commitment to recruit 6,000 new GPs, given the overall context of rocketing demand for GP services, with our ageing, longer-lived population meaning there are larger numbers of people with serious health needs than ever before. To meet this, ministers are injecting nearly £1 billion more per year into the core GP contract, as part of an overall increase of £33.9 billion in the annual NHS budget.
Rachael Maskell, Labour MP for York Central

Rachael Maskell
Primary care is underfunded and therefore York is comparatively worse off than much of the country"
Any GP would say, that before you deliver the medicine, you need a diagnosis. The GP crisis has been building for a significant period of time and there are certainly solutions.
York has historically fared poorly under the NHS funding formula, which has meant that primary care is underfunded and therefore comparatively worse off than much of the country, which is also significantly underfunded and understaffed.
The number of patients per practice has risen by 22 per cent since 2015, yet the number of GPs has been broadly static with just 0.46 GPs per 1000 in England (down from 0.52 in 2015). Currently practice appointments are up 18 per cent compared to a year ago, with GP appointments up 15 per cent according to the BMA. Next-day appointments are the highest on record.
With the NHS having to find capacity to support five million people waiting for appointments and procedures, it is often local surgeries which counsel and help patients while they wait.
GPs themselves are also ageing and retiring, and after this last year, are certainly planning their futures as there is only so much mental exhaustion, long hours and constant stress and pressure that anyone can take.
Others have been helping out at the vaccine hub giving us all the hope and protection we need to return to some form of normality.
Our GPs, who have worked relentlessly over the last year, have innovated service delivery by using digital technology to consult with patients and support them with managing their conditions, as ‘expert patients’.
Others have diversified their clinical teams, subsidising a GP-only service with nursing practitioners, physios, mental health staff and other key workers. York is pioneering social prescribing to support the wider challenges of ill health.
But we cannot shy away from the patient experience. The frustrations by which people have come to me demonstrates that access to healthcare is not working.

Patients are waiting for a long time on the telpehone to make a GP appointment
As we have seen with the vaccine programme, when minds come together solutions can be found. We need to build on this learning and ensure that all GPs work as one, that there is a system that builds on the breadth of clinical and non-clinical skills to administer, triage, diagnose and treat patients in a fair and timely way.
As with the pandemic, we have accepted that we go to central locations to receive tests and vaccines. While, of course, people will forever need their local GP surgeries, if the rest of the population in this recovery phase of the NHS would use more systematic primary care services, we have an opportunity to start recovering a GP service and building it differently, and even better than before.
We all have to accept that Covid-19 was only one part of the health crisis, but after a decade of starvation of funding, rationing and cuts, we have to also accept that there have been serious consequences.
Privatisation and fragmentation has broken the NHS.
The NHS was built to stand as one system to care for patients, and I would urge the CCG to start trusting GPs more and withdraw from commissioning from profit-making bodies. We must find NHS solutions to health challenges as we all would want.
Finally, we have to invest in better public health. It will only be when we live healthier lives that we will be able to thrive and have less dependency on our GPs in the future.
What's your view? Write us a letter - email: letters@thepress.co.uk
Please write no more than 250 words and provide your name, address and telephone number






Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel