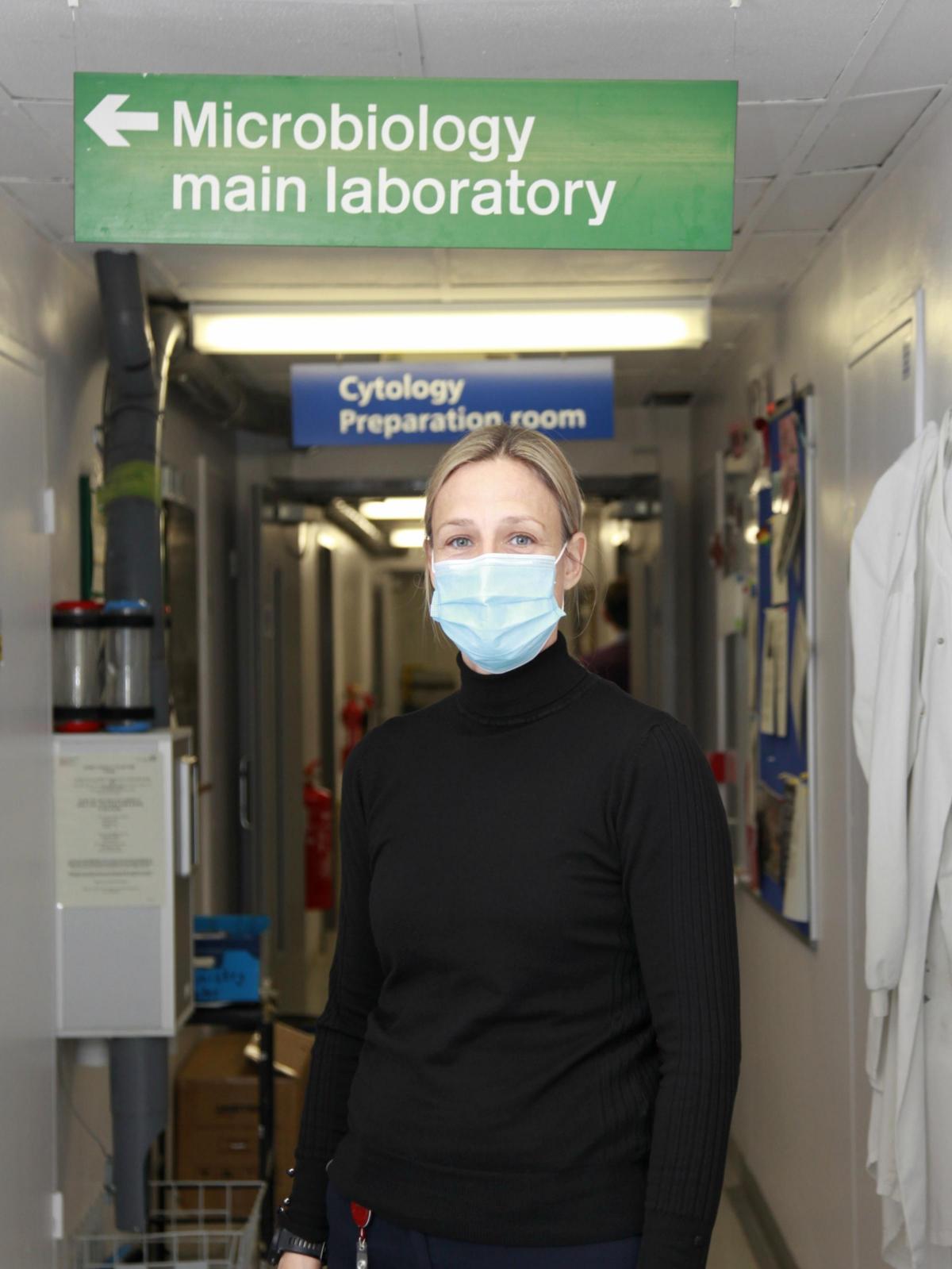
Most people who visit York Hospital will never come across Lisa Mead and her team in the microbiology labs.
Chances are you won’t even know they’re there.
But throughout the coronavirus pandemic they have played a vital part in enabling the hospital to keep treating patients.
It is Lisa and her team who test swab samples from staff and patients alike to see whether they have coronavirus or not.
All patients who are due to be admitted to hospital for a planned procedure such as an operation are tested for the virus first. Inpatients who have been in hospital for some time are also re-tested after 5-7 days.
And any staff who develop symptoms can quickly access a swab test to determine whether or not they have Covid-19.
Lisa and her team can turn those swab tests around in a matter of just a few hours. It’s a vitally important job.
“We need to know whether people are positive or not,” says Lisa, 45, the hospital’s head biomedical scientist. “It’s about enabling surgery to continue.”
Given that the Covid-19 virus is so infectious, even testing samples carries a risk.
But Lisa and her team are used to dealing with some very nasty bugs indeed - everything from bacteria such as MRSA, campylobacter and salmonella to viruses like HIV and hepatitis.
The microbiology labs on the hospital’s first floor include a ‘containment level 3’ (CL3) lab where samples which might contain the worst nasties - ‘Hazard Group 3’ or HG3 pathogens which can cause severe human disease and can spread rapidly if they get out - are analysed.
The lab has sealed doors and windows and is held under ‘negative pressure’ - the air pressure inside is slightly lower than outside, so if a door is opened, air comes in rather than going out.
Air is passed through double filters, and access to the lab is strictly restricted. “Nothing can escape,” Lisa says.
Within the CL3 lab staff wear special lab coats, facemasks and eye shields, gloves, and cuffs on their sleeves. Clothing is sterilised every day, and all waste samples are sterilised at high temperatures and pressures in a piece of kit known as an autoclave before being disposed of as medical waste.
It is the kind of highly secure lab that you might see scientists working in on a TV series about a virus outbreak. And it is here that swab samples from patients and staff at York Hospital are brought for testing.
Samples are taken from the nose and throat of those being tested by hospital staff. They’re immediately placed in a liquid suspension in a tiny sealed container which is then ‘double bagged’ for extra security.
When the samples arrive at the CL3 lab they are ‘deactivated’ by heat treatment so scientists can handle them safely.
They’re then put through a complex process of chemical reactions in the lab to look for evidence of Covid RNA (a molecule similar to DNA which carries the genetic code of the virus).
If Covid RNA is present, it means the person from whom the swab sample was taken is Covid-positive. It is a process known as a polymerase chain reaction (or PCR) test, which is highly sensitive to any Covid RNA, Lisa says.
The results come through in 5-6 hours at most (and sometimes as quickly as in a couple of hours) and are immediately communicated to medical teams on the wards.
As York Hospital Trust’s head biomedical scientist, Lisa is in charge of about 65 staff across two hospitals, in York and Scarborough.
When the coronavirus pandemic first reached these shores, her department didn’t have the testing kit needed to test Covid swab samples. In those first few weeks, swab samples from York all had to be sent to public health labs in Leeds for analysis.
The first piece of kit (an MT Prep analyser) arrived in March, with a second, similar instrument being delivered in June. Now the Trust’s labs have the capacity to do limited rapid Covid testing, too - in which the results are available in just a couple of hours.
Because of the expected surge in coronavirus cases, extra staff are being taken on - eight in York and four in Scarborough. Lab staff have also done extra training.
Her staff are ready, Lisa says. “We could not be more prepared. Bring it on!”
She and her staff are used to dealing with dangerous pathogens.
Long before Covid reared its ugly head, they played a vital role in analysing patient samples for evidence of a range of nasty germs: antibiotic resistant bacteria such as MRSA (which causes lung infections and blood poisoning) and C. difficile (severe diarrhoea); the bacteria which cause food poisoning, such as salmonella and campylobacter; HIV and hepatitis viruses; and some nasty fungal diseases.
When they find evidence of bacterial infections, they can quickly test them with various antibiotics to see which are likely to work best - information that is hugely useful to medics treating patients.
They also notify public health officials about key pathogens - enabling them to keep track, for example, of the development of antibiotic resistance.
That’s a problem that is likely to be with us long after the coronavirus is over.
It’s a threat that gives nightmares to experts such as Professor Colin Garner, who heads up York-based charity Antibiotic Research UK.
He’s gone on record as saying that modern medicine as we know it would become almost impossible if antibiotics stop working. Simple operations - hip replacements or even tooth extractions - would become much more risky, because of the danger of infection.
Lisa is aware of the risk. “It is something that, perhaps not in my lifetime, but maybe...” Her voice trails off.
The microbiology lab’s work in testing for all these dangerous nasties continues.
But for now at least, it is coronavirus that remains the key challenge.
Wearing PPE and taking hygiene precautions is nothing new for Lisa and her team.
But what is different is the sheer scale of what is happening.
“I never thought I would experience a pandemic, and be able to do what we’re doing now for the city of York,” she said. “It is a challenge, but it is also an experience we will never forget.”
And is she herself personally worried about the virus?
No, says the married mum of one grown-up daughter. And for a very simple reason. “We follow the rules,” she says - meaning the rules on social distancing and hygiene.
If the woman who spends her life dealing with nasty bugs thinks it is important to stick to those rules - well, then you can take it as read that it’s important.
Remember that next time you're tempted to break the rules...
York Hospital coronavirus update
At time of writing, there were 34 Covid-positive patients at York Hospital, being looked after on two specially-designated Covid wards.
Since the pandemic began, there had been 229 Covid-related deaths Trust-wide at the hospitals in York and Scarborough.









Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel